Introduction
Diabetic retinopathy is a major cause of vision loss in adults of working age around the world. This eye disease gets worse over time because high blood sugar levels hurt the blood vessels in the retina, which is the light-sensitive tissue at the back of the eye. Fortunately, modern treatments have made a big difference in the results, especially when the disease is found early. Patients can make better choices about their eye care and keep their vision by learning about these treatment options.
What is Diabetic Retinopathy?
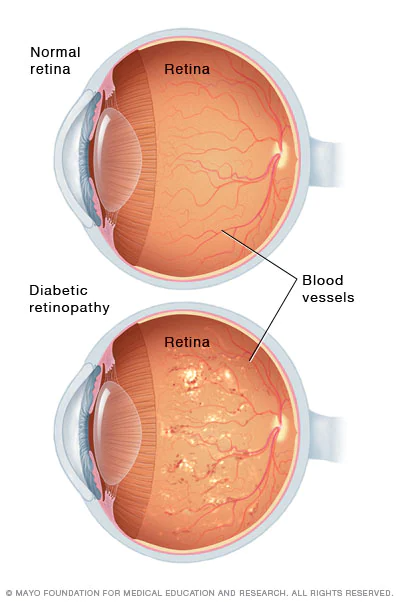
Before looking into treatment options, it’s important to know how diabetic retinopathy gets worse. There are two main stages of the disease: nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). In the early stage of NPDR, blood vessels that are damaged leak fluid and form microaneurysms. PDR, the more advanced stage, is when new blood vessels grow that aren’t normal and can cause bleeding and scarring. Different treatments are used depending on how far along the disease is and the person’s own situation.
Conservative Management and Prevention
The basis of diabetic retinopathy treatment commences with prevention and meticulous disease management. Keeping blood sugar levels under strict control is the best way to stop or slow the progression of retinopathy. Studies have consistently demonstrated that patients who attain and sustain optimal glycemic control markedly diminish their risk of developing retinopathy or experiencing vision impairment.
Also, keeping blood pressure and cholesterol levels in check is very important for slowing the progression of disease. Regular eye exams, at least once a year for people with diabetes and more often if retinopathy is found, help doctors find changes early. For patients with mild to moderate NPDR and no macular edema, careful observation along with good control of systemic disease may be enough, as long as they are checked regularly to see if the disease is getting worse.
Injections of anti-VEGF
Anti-vascular endothelial growth factor (anti-VEGF) drugs are a big step forward in the treatment of diabetic retinopathy. These drugs stop VEGF, a protein that makes blood vessels grow in strange ways and makes them more permeable. Bevacizumab, aflibercept, and ranibizumab are three common anti-VEGF drugs.
These drugs are given as intravitreal injections, which means they are injected directly into the vitreous humor of the eye. Most of the time, patients get injections once a month or once every other month, depending on the drug and how their body reacts. Anti-VEGF therapy is especially good at treating diabetic macular edema (swelling in the macula, the central part of the retina) and can stop or even reverse vision loss in many cases. Many eye doctors now think that anti-VEGF therapy is the best first-line treatment for diabetic macular edema because studies have shown that it works better than older laser treatments alone.
Injections of corticosteroids
Corticosteroid drugs can help with swelling and make blood vessels in the retina less permeable. Intravitreal corticosteroid injections, including triamcinolone acetonide and implantable dexamethasone devices, are occasionally employed to manage diabetic macular edema, especially when patients do not adequately respond to anti-VEGF therapy or possess contraindications to these medications.
Corticosteroids and anti-VEGF drugs work in different ways, and in some cases, they can be used together for the best results. The length of time that the effect lasts varies; some formulations give relief for a few months, while others are made for long-term use. Possible side effects, like higher pressure in the eye and the formation of cataracts, need to be watched closely.
Photocoagulation with a laser
Laser photocoagulation is still an important tool for managing diabetic retinopathy, even though it is not as commonly used as a first-line treatment anymore. This procedure uses a focused laser beam to make small burns on the retina. It is usually used to treat areas where blood vessels are growing abnormally or the retina is swelling.
During pan-retinal photocoagulation (PRP), many small burns are made on the retina to lower the amount of oxygen it needs and stop the growth of new blood vessels. This procedure is still the best way to treat advanced proliferative retinopathy, especially when new blood vessels are threatening the optic nerve or when anti-VEGF therapy can’t be used. Focal laser treatment focuses on certain areas of macular edema and can be used with other treatments. Laser treatment has a lot of drawbacks and side effects compared to newer methods, but it is still useful in some clinical situations.
Surgery for vitrectomy
If a person has severe proliferative retinopathy, a lot of bleeding in the eye (vitreous hemorrhage), or advanced fibrosis and scarring, they may need vitrectomy. This surgery involves taking out the vitreous gel from the eye so that the surgeon can get to the retina and treat it directly. The surgeon can get rid of scar tissue, fix retinal detachments, and stop bleeding vessels during the procedure.
Vitrectomy is a more invasive procedure than injection therapies, but it can save vision in advanced cases and can be used with other treatments. Surgical techniques and tools have improved, making vitrectomy safer and more effective. It also helps people see better faster than it used to.
New and extra treatments
Researchers are still looking into other ways to treat people. Some patients may do better with intravitreal steroids and anti-VEGF agents together. Researchers are looking into new drugs that work on different pathways in retinal inflammation and vascular dysfunction. Researchers are looking into oral medications and supplements, but there isn’t much evidence yet.
Also, better imaging technologies like optical coherence tomography (OCT) make it easier to keep an eye on changes in the retina and plan treatments more accurately. Some patients may benefit from visual aids and low-vision rehabilitation services to make the most of what vision they still have.
Results and Expectations of Treatment
The outlook for diabetic retinopathy has improved greatly in the last twenty years. A lot of people who get modern treatments keep or even improve their vision. But the results depend on a number of things, such as the stage of the disease when it first shows up, how well the patient follows treatment guidelines, how well the disease is controlled in the body, and how each person responds to treatment differently.
After just one injection or laser treatment, patients usually don’t feel better right away; they usually need more than one session. The goal of treatment is to stop the disease from getting worse and stop more vision loss, but it isn’t always possible to fix major damage. Regular follow-up appointments are important to keep an eye on how well the treatment is working and make changes to the management plan as needed.
The Importance of Finding and Stopping Problems Early
Although advanced treatments exist, prevention is the most effective approach. People with diabetes should keep their blood sugar levels in check, their blood pressure and cholesterol levels in check, their weight in check, and their smoking habits in check. Ophthalmologists can find retinopathy early, when treatment is usually more effective and vision is more likely to be preserved, by doing full eye exams every year.
Conclusion
Treatment for diabetic retinopathy has come a long way and now includes many evidence-based options that are tailored to each patient’s needs. The goal of today’s treatment is to protect vision and improve quality of life, from conservative management that focuses on glycemic control to advanced anti-VEGF injections and surgery. To be successful, the patient and their healthcare team need to work together to find the best way to manage the disease and treat the eyes. People with diabetes should get their eyes checked regularly and work hard to control their disease. This will help their vision health in the long run.